Private CAMHS and young people's services
Call today for more information about how Priory help children and young people who are struggling with their mental health.
There's no doubt that growing up can be an emotional rollercoaster for many young people, and it can be difficult for a parent or carer to identify when a child’s behaviour is related to a mental health condition, and when they may need specialist help and support.
CAMHS, short for child and adolescent mental health services, is a service that offers support and treatment to young people who are struggling with a range of mental health conditions. Another term used to describe a service that aids young people is CYPMHS, or children and young people's mental health services.
Our exceptional young people’s wellbeing services at Priory are comprised of highly skilled child psychiatrists, psychologists, therapists and other mental health professionals, many of whom are published experts in their field.
Priory’s specialist team, coupled with our extensive national network of mental health hospitals and wellbeing centres, mean that we're extremely well-placed to deliver world class treatment, in a location that is convenient for you.
We offer fast assessment and treatment to children, young people and families, for those aged under 18.
At Priory, we can offer fast access to services for children and young people who:
While we’re not an emergency service at Priory, we’re dedicated to your onward recovery and stabilisation, and will help you to get back on track. Our highly trained mental health treatment experts will help you to understand your issues, and support you every step of the way towards a healthier and more positive future.
All of the treatment provided as part of our private CAMHS offering is flexible, and can be tailored to each person’s specific needs and personal circumstances. We offer:
A range of treatment programmes that can be either scaled up or scaled down according to the intensity of the support that's needed. These include:
Tried and tested therapy types including:
Therapy delivered in a number of different formats including:
If you know a child who's struggling, our experts are here to help. We're able to offer a range of private CAMHS assessments, including attention deficit hyperactivity disorder (ADHD) and sensory assessments, as well as specialist educational assessments such as the Wechsler Intelligence Scale for Children (WISC).
Our experts also offer evaluations for autism, as well as mental health conditions like depression, anxiety, and psychosis. Learn more about our autism assessments here.
Our private CAMHS assessments are possible without the need for a GP referral, without having to join a waiting list, and without having to pay for a psychiatric assessment as a first step to accessing our services.
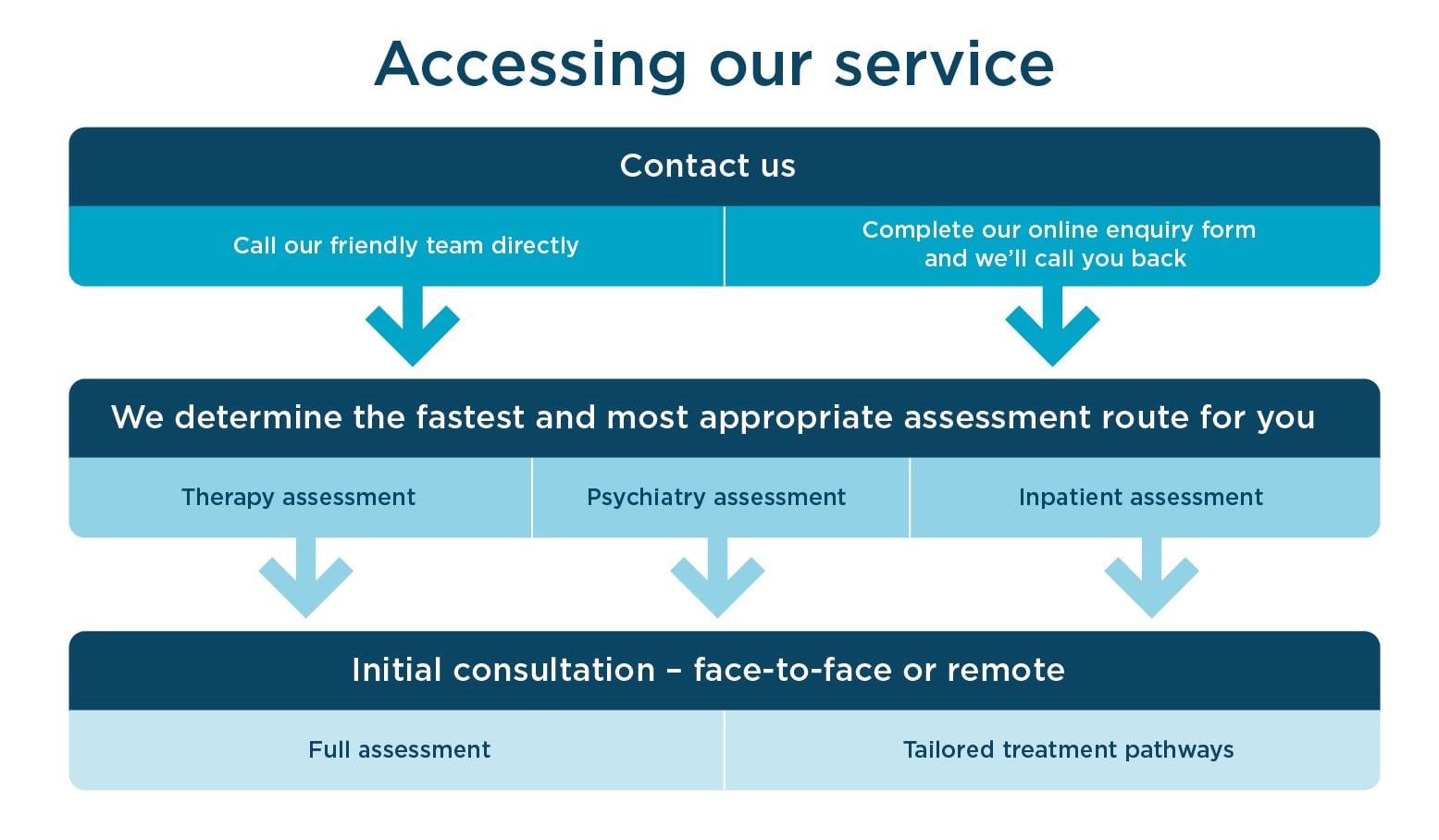
If you’re worried about a child, it’s important to get in touch right away. You can call us using our CAMHS contact number, 0330 056 6041, or alternatively you can submit an online enquiry form and one of your team will be in touch shortly.
There are many reasons someone may choose a private healthcare service over a publicly funded service. Just some of these reasons include:
It’s important to remember that young people, parents and caregivers don’t have to struggle alone; expert psychiatric support for children and adolescents is available, and the most crucial first step is to seek specialist treatment.
Using a comprehensive range of evidence-based therapy programmes, and having leading experts in child and adolescent psychiatry, our exceptional young people’s services are dedicated to providing the best possible mental health support for children and young people.
At Priory, we offer tried and tested treatment for a range of mental health conditions presenting in children and young people. These include:
The initial call with our customer service centre only takes a few minutes. Once you've been allocated to an assessment with one of our specialist team, this initial consultation takes between 60 to 90 minutes.
We always prefer to meet families face-to-face, but we also offer the convenience of meeting with you remotely, so you can be in the comfort of your own home.
We don’t always need a GP referral, but we’ll ask for consent to contact your GP as part of your treatment.
The cost of the initial assessment for a young person starts from £186. This includes a 60-minute virtual session with one of our specialist and highly-trained psychologists or therapists, as well as a detailed summary report. Following this, we'll provide our recommendations for further treatment, which may include a private psychiatry assessment.
For more information, please visit our getting started page or call our friendly team.
We're all specialists providing evidence-based care, and very often, we work together to provide you with the best treatment.
Psychologists provide evidence-based talking therapies, they have a psychology degree and are trained to provide psychological testing and treatment.
Therapists, or psychotherapists, can be from a variety of care backgrounds. The word ‘therapist’ is a generic term that can refer to a counsellor, clinical psychologist, family therapist, integrative therapist, or someone specialising in only one type of therapy, such as cognitive behavioural therapy (CBT).
Psychiatrists are medically qualified doctors, specialising in mental health. Psychiatrists often hold an overview of someone’s care, provide diagnostic testing and medication where needed.
Don’t worry if you don’t know which specialist you need; we'll determine the most appropriate specialist for you to see.
You can read more about the differences between counsellors and therapists here.
Along with the everyday struggles that mental health difficulties can bring, they can also prevent young people from achieving their best in school. Many schools make contact with Priory to discuss how we can support staff, pupils and their families in managing mental health challenges within an educational context.
We are able to offer bespoke support packages for schools, and welcome enquires from those wishing to promote a culture of positive mental health within their school and ultimately, help their students to better manage their mental health. To find out more about our school support offering, contact us today on 0800 098 4829.
Priory’s customer service team is available 24 hours a day, 7 days a week to ensure that people in crisis can be signposted to the best possible support. The specialist teams at our residential facilities can help to stabilise people in need of assistance for their mental health concerns.
If your GP is willing to enter a shared care agreement, we can organise this for the young person under the care of a Priory psychiatrist. This usually means that your GP will issue prescriptions while you remain under the specialist supervision of a private CAMHS psychiatrist.

We are a registered and approved provider for all of the UK's leading private medical insurers. Many of the services we offer at Priory can be funded through private medical insurance. This includes:
All clients will have access to our highly skilled and accredited clinicians, many of whom are published experts in their fields of treatment. Whatever your requirements, we are committed to working with you to get your life back on track.
We have CAMHS treatment centres located throughout the country, meaning that you can access the support you need in a location that’s convenient for you. To find your nearest CAMHS treatment centre, please use the search form below.