What causes depression?
Depression can arise from a variety of causes, but understanding the factors at play is the first step toward recovery.
Depression is a complex condition that rarely has a single cause. It usually develops through a combination of biological, psychological and social factors, each influencing the other.
Understanding what might be contributing to how you feel can be an important step towards getting better. It’s not your fault, and with the right support, recovery is possible.
Depression often arises when biological, psychological and social factors interact. For example, someone with a genetic vulnerability might experience depression after a major life stressor, while another person might develop it following a physical illness or prolonged stress.
These factors don’t determine your future, they simply highlight areas where support and treatment can make a difference.
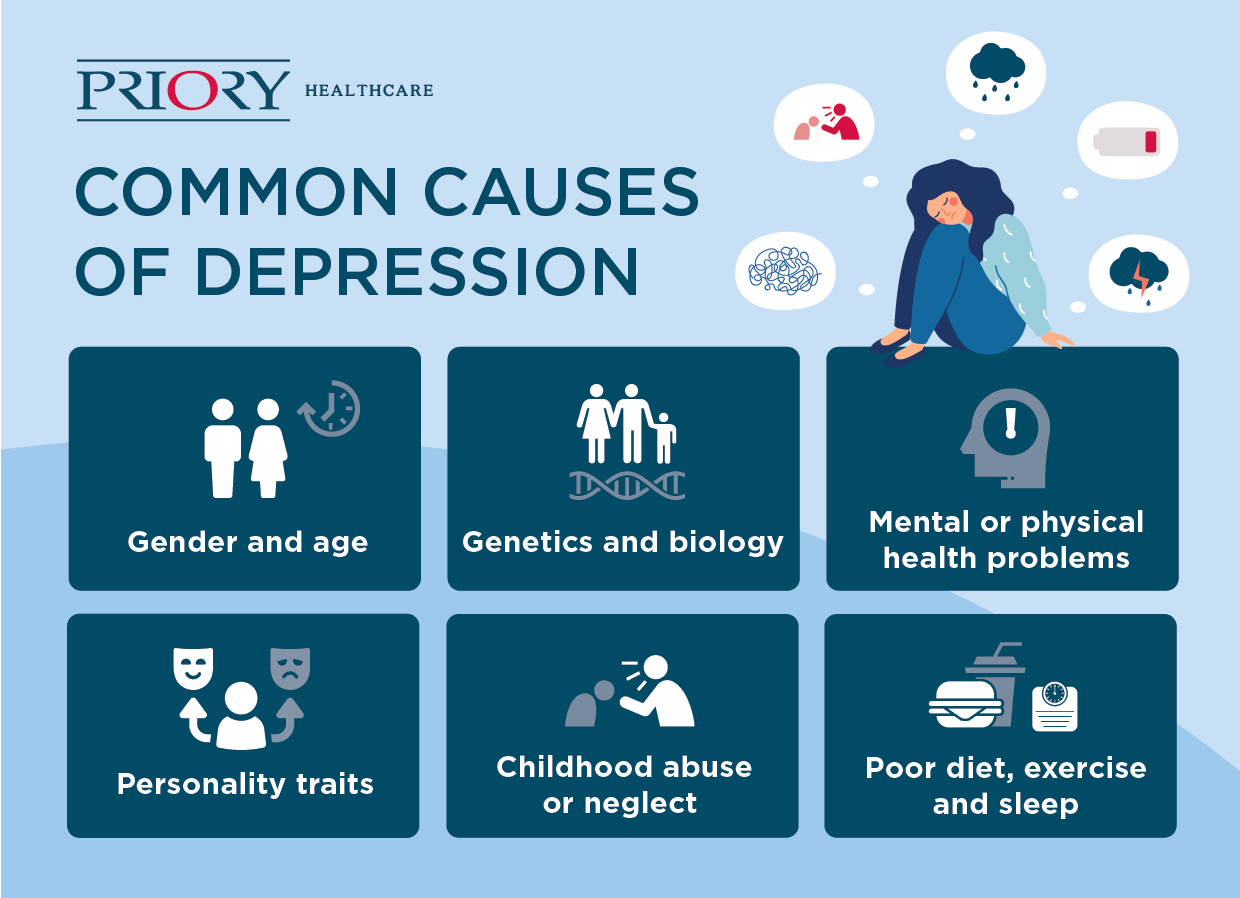
Depression can run in families, but it isn’t purely genetic. Having a parent or sibling with depression may increase your vulnerability, but it doesn’t mean you’ll develop it too. Environment, lifestyle and coping strategies also play important roles.
Depression is linked to changes in the brain’s communication systems. Neurotransmitters such as serotonin, dopamine and noradrenaline help regulate mood, sleep and motivation. When these are disrupted, it can affect how you feel and think.
Hormonal shifts, for example, during menstruation, pregnancy, menopause or as a result of thyroid disorders, can also influence mood and energy levels.
Long-term or serious illnesses can affect both body and mind. Conditions like chronic pain, diabetes, heart disease and neurological disorders are known to increase the risk of depression. Some medications can also contribute to low mood.
Tip: If you’re worried that depression medication might be affecting your mood, speak to your GP or pharmacist before making any changes.
Certain thought patterns or personality traits can make some people more prone to depression. These may include perfectionism, self-criticism or a tendency to dwell on negative thoughts. Low self-esteem or feeling unable to manage stress can also contribute.
Difficult or traumatic experiences, particularly in childhood, can increase vulnerability to depression later in life. This can include abuse, neglect, bullying or significant loss. Conditions such as post-traumatic stress disorder (PTSD) and complex PTSD (CPTSD) often involve depressive symptoms.
People sometimes cope with distress through avoidance, overworking, or using substances like alcohol or drugs. While these might offer temporary relief, they often worsen low mood over time.
Therapies such as cognitive behavioural therapy (CBT), dialectical behaviour therapy (DBT) and trauma-focused therapy can help identify and rework these patterns.
Major life changes or ongoing pressures can have a significant emotional impact. Common examples include:
Lack of sleep, low physical activity and poor nutrition can all influence brain chemistry and mood. Alcohol or recreational drug use can also disrupt emotional balance and increase depressive symptoms.
Seasonal changes
For some people, depression appears during the darker months when daylight hours are shorter, known as seasonal affective disorder (SAD). Light exposure, maintaining a routine and professional support can all help manage these effects.
Depression often develops when a trigger interacts with an existing vulnerability, for example, stress at work in someone who already has low self-esteem, or illness in someone with a family history of depression.
While you can’t always control vulnerabilities, you can learn to manage triggers and build resilience through therapy, lifestyle changes and professional support.
Bullying, academic pressure and family conflict can contribute to depression in young people. Symptoms may appear as irritability, withdrawal or physical complaints rather than sadness.
Hormonal changes, sleep deprivation and major life adjustments after childbirth can lead to perinatal depression. Both parents can be affected, not just mothers.
During menopause, fluctuating hormone levels can affect mood and energy. The right support and treatment can make these changes easier to manage.
Loneliness, bereavement and chronic health problems can make older adults more vulnerable to depression. Depression in later life is often overlooked, but it is highly treatable.
Men may show irritability, anger or increased risk-taking rather than sadness, while women may experience more guilt or rumination linked to hormonal influences.
If you recognise some of these risk factors or triggers in your life, remember that depression is treatable and help is available.
You should seek support if:
In an emergency:
Call 999, go to your nearest A&E, or contact Samaritans on 116 123 (free, 24/7).
Next steps:
At Priory, we offer evidence-based treatment for all forms of depression. Our services include:
Take the first step towards feeling better, book a confidential assessment today.